
You may have had “butterflies in your stomach” during anxious or stressful moments. These phrases are not merely metaphors—your gut and brain connection is profoundly real. There is a bidirectional communication (two-way communication) network between your gut and brain, known as the gut-brain axis. That plays a vital role in your mental health, feelings, and behavior.
Recent advances in science have led researchers to suggest that your gut microbiome (the trillions of microorganisms living in your digestive tract) not only plays a role in digestion but also communicates with your brain via various hormonal, immune, & neural routes. This gut and brain connection has created interest among researchers from a range of fields, including neuroscientists, psychologists, and gastroenterologists.
Take care of your gut health with our comprehensive range of stomach care products. Browse Stomach Care Products
What is the Gut-Brain Axis?
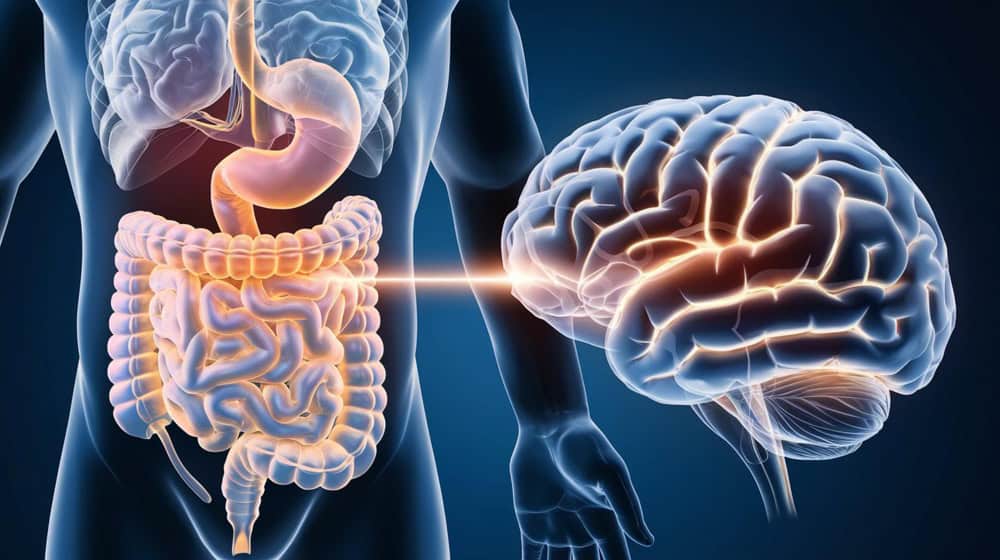
The gut and brain connection defines the two-way communication pathway between the central nervous system (CNS) & the enteric nervous system (ENS), which is responsible for regulating the gastrointestinal (GI) tract. The two-way communication pathway can happen in a variety of ways:
-The vagus nerve directly connects the gut and brain
-Signals sent through the immune system
-Channels made by microbial metabolites
-Hormonal and neurotransmitter pathways
The gut is often called your body’s “second brain” because it contains over 100 million neurons (more neurons than the spinal cord). It has such a powerful network of neurons that it can function independently of the brain[1].
Impact of Gut Health on Mental Health

There is a growing consensus that gut microbiota affects various aspects of mental health. Many mental health problems, including depression, anxiety, autism, and Alzheimer’s disease, are related to dysbiosis (an imbalance of the gut microbiome), which in turn disrupts the gut and brain connection.
1. Depression & Anxiety

In a study, researchers demonstrated how individuals diagnosed with major depression presented a significantly different gut microbial population compared to healthy individuals [2]. Furthermore, probiotics have been found to help lessen the degree of severity of depressive symptoms [3].
2. Stress Response

The gut and brain connection influences the hypothalamic-pituitary-adrenal (HPA) axis (controlling your stress response). Animal studies have shown how germ-free mice (mice raised without gut bacteria) experience excessive HPA axis response to stress but are cured when healthy bacteria are added [4].
3. Cognitive Function

Short-chain fatty acids (SCFAs), such as acetate and propionate, reduce inflammation, improve memory, and strengthen the blood-brain barrier (BBB). A 2025 study published in Nature established that by modifying the gut microbiota in mice, laboratory measures of spatial learning and memory improved, again underscoring the importance of a strong gut and brain connection [5].
Diet and Gut-Brain Health

Your diet can affect the diversity and richness of your gut microbiome and can impact brain function via the gut and brain connection. Here’s how:
-Foods high in fiber, such as legumes, oats, fruits, and vegetables, nourish good gut bacteria and stimulate SCFA (short-chain fatty acids).
-Fermented foods such as yogurt, kimchi, kefir, and miso contain probiotics that can help you.
-Foods high in polyphenols, such as berries, green tea, and cocoa, have prebiotic-like effects and promote microbial health.
-On the other hand, ultra-processed foods and sugary diets promote dysbiosis and inflammation.
-In a study, investigators found that a Mediterranean diet was associated with a lower risk of depression and was consistent with a diet enriched in both fiber and healthy fats [6].
Gut Health and Neurodegenerative Disorders

Few researchers are exploring whether gut microbiota may influence the incidence of Alzheimer’s disease and Parkinson’s disease. Inflammation in the gut may be a source of neuroinflammation, a prominent factor in the incidence of these disorders [7].
In patients with Parkinson’s disease, scientists have noted the ability of certain gut microbes to produce proteins that resemble alpha-synuclein. These proteins may travel to the brain via the vagus nerve, resulting in the deposition of toxic proteins characteristic of Parkinson’s disease [3].
How to Help Your Gut-Brain Axis

A healthy gut can support your brain health and restore the gut and brain connection. Here are a few ways to improve your gut based on sound evidence:
-Eating a varied, plant-based diet: The gut microbiota prefers a diverse diet containing lots of plant matter because it enhances the diversity of microbial species and has the potential to improve short-chain fatty acid production.
-Include prebiotics and probiotics: Probiotics such as Lactobacillus and Bifidobacteria can positively influence mood states. Also, prebiotics such as inulin and resistant starch feed the beneficial microbes.
-Manage your stress: Chronic stress can damage the gut lining and disturb the microbial community. Use mindfulness, deep breathing, and regular exercise to manage stress.
-Get plenty of quality sleep: Sleeping well allows the gut bacteria to reset, and gut bacteria can also influence mood states and cognition.
-Avoid taking antibiotics unnecessarily: Antibiotics can save lives, but they have the side effect of killing the good gut bacteria. When using antibiotics, be diligent in their use and speak to your healthcare provider about any concerns.
You can consult a doctor from the comfort of your home. Schedule an appointment today with a click.
Final Thoughts
The gut microbiome plays a key role in how you feel, think, and behave daily. By taking care of your gut health (via diet, lifestyle, and mindfulness), you can improve your mental health and cognitive function.
As researchers continue to look at this rich relationship, one thing is crystal clear: a healthy gut equals a healthier mind.
FAQs
Q. Can poor gut health cause anxiety or depression?
Yes, poor gut health can lead to anxiety or depression. Studies report that a state of gut dysbiosis (an imbalance of bacteria in the gut) is associated with increased rates of depression, anxiety, and stress that result from inflammation and alterations in neurotransmitter production, such as serotonin and GABA.
Q. What foods support gut-brain health?
Fiber-rich foods, fermented foods including yogurt and kimchi, foods high in polyphenols including berries and green tea, prebiotics, and probiotics. These foods support a healthy gut microbiome that positively influences brain function through the gut and brain connection.
Q. Do probiotics improve mental health?
Some strains of probiotics, also called psychobiotics, have been studied for their potential to reduce symptoms of depression and anxiety by improving gut health and regulating the Human Stress Response System (HPA-axis).
Q. Does the gut and brain connection influence memory?
Yes, a healthy gut–brain connection supports learning and cognition. Short-chain fatty acids produced by gut microbiota help decrease inflammation in the body and support memory, learning, and attention.
Q. Can dysfunction in the gut and brain connection lead to mental health conditions?
Yes, dysfunction in the gut and brain connection has been linked to anxiety, depression, and even neurodegenerative diseases related to the disturbance of microbiota and inflammation.
Recommended Reads
5 Foods For Better Gut Health Digestion
(The article is written by Deepa Sarkar, Medical Writer, and reviewed by Monalisa Deka, Senior Health Content Editor)
References
1. Woo C. Our second brain: More than a gut feeling [Internet]. UBC Neuroscience. 2020 [cited 2025 Jun 26].
2. Jiang H, Ling Z, Zhang Y, Mao H, Ma Z, Yin Y, et al. Altered fecal microbiota composition in patients with major depressive disorder. Brain Behav Immun. 2015;48:186–94.
3. Sarkar A, Lehto SM, Harty S, Dinan TG, Cryan JF, Burnet PWJ. Psychobiotics and the manipulation of bacteria–gut–brain signals. Trends Neurosci. 2016;39(11):763–81.
4. Sudo N, Chida Y, Aiba Y, Sonoda J, Oyama N, Yu XN, et al. Postnatal microbial colonization programs the hypothalamic–pituitary–adrenal system for stress response in mice. J Physiol. 2004;558(Pt 1):263–75.
5. Ahn J-S, Kim S, Han E-J, Hong S-T, Chung H-J. Increasing spatial working memory in mice with Akkermansia muciniphila. Commun Biol [Internet]. 2025 [cited 2025 Jun 26];8(1):546.
6. Radkhah N, Rasouli A, Majnouni A, Eskandari E, Parastouei K. The effect of Mediterranean diet instructions on depression, anxiety, stress, and anthropometric indices: A randomized, double-blind, controlled clinical trial. Prev Med Rep [Internet]. 2023;36(102469):102469.
7. Sampson TR, Debelius JW, Thron T, Janssen S, Shastri GG, Ilhan ZE, et al. Gut microbiota regulates motor deficits and neuroinflammation in a model of Parkinson’s disease. Cell. 2016;167(6):1469–80.e12.