Wilson's disease
Wilson’s disease is a rare inherited condition in which the body can’t clear excess copper. Instead, this copper slowly accumulates in the liver, brain, and eyes, where it begins to cause damage. The primary cause is a defective gene that is inherited from both parents and interferes with the body's natural process of expelling copper through bile.
Anyone with this gene is susceptible, and siblings of an afflicted individual are more likely to get it. Symptoms typically appear in childhood or young adulthood, but the age and timing can vary. People may experience tiredness, jaundice, mood swings, shaky hands, or balance issues as copper levels rise.
Long-term medications that either remove excess copper or prevent it from building up are part of the treatment. With early diagnosis and consistent care, most people can lead healthy, active lives.
- Age group 6-45 years
- Both men and women more common in women
- Liver
- Brain
- Eyes
- Neuroacanthocytosis syndromes
- Huntington's disease
- Sydenham chorea
- Primary biliary cholangitis
- Heavy metal poisoning
- Alcohol-related liver disease
- Alcohol-associated hepatitis
- Zieve’s syndrome
- Viral hepatitis
- Evan’s syndrome
- Parkinson’s disease
- Blood and urine tests: Liver function tests, INR (International Normalised Ratio) & albumin, Ceruloplasmin, Red blood cells (RBC) and Urine copper test
- Genetic testing
- Liver biopsy
- Imaging tests: Brain MRI, Ultrasound or transient elastography
- Leipzig scoring system
- General physician
- Paediatrician
- Hepatologist
- Neurologist
- Clinical geneticist
- Gastroenterologist
Symptoms of Wilson’s Disease
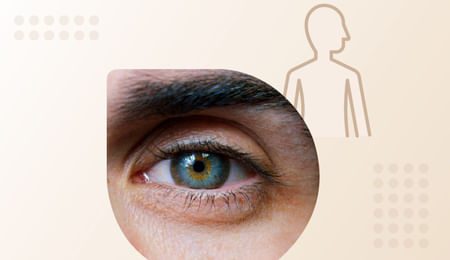
Wilson’s disease usually starts in childhood or the teen years, but it can show up even later in life. One key sign is the Kayser–Fleischer ring—a rusty brown ring around the eye that doctors can see during an eye exam. It doesn’t affect vision but signals copper buildup in the body.
The rest of the symptoms vary depending on which organs are affected, such as the liver, brain, or muscles.
Liver-related symptoms (common in children)
-
Jaundice (yellow eyes/skin)
-
Swelling in the legs or abdomen
-
Easy bruising or bleeding
-
Fluid in the belly (ascites)
-
Abnormal liver tests, or sudden liver failure
-
Scarring of the liver (cirrhosis)
Neurological symptoms (more common in teens and adults)
-
Tremors or shaky hands
-
Slurred speech
-
Difficulty swallowing
-
Poor balance or coordination
-
Muscle stiffness or abnormal postures
-
Kayser–Fleischer rings- a rusty brown ring around the eye
Brain-related symptoms
-
Mood or personality changes
-
Trouble concentrating
Reproductive symptoms (especially in young women)
-
Irregular or absent periods
-
Difficulty conceiving or repeated miscarriages
Other rare symptoms:
-
Bone and joint problems ( arthritis or osteoporosis)
-
Bone spurs near large joints
-
Joint stiffness or joint pain
-
Kidney tube damage increases the risk of kidney problems or even kidney failure.
-
Heart problems like weak heart muscles or abnormal heart rhythms
Causes of Wilson’s Disease
-
Wilson’s disease is caused by a mutation in the ATP7B gene, which normally helps the body get rid of excess copper.
-
In a healthy body, the liver sends extra copper into bile, a digestive fluid stored in the gallbladder. Bile then carries copper and other waste out of the body through the digestive system.
-
Because the liver is unable to adequately release copper into bile in Wilson's disease, excess copper accumulates in the body and gradually damages organs like the brain and liver.
Risk Factors for Wilson’s Disease
You are at higher risk if your parents or siblings have Wilson’s disease. Other things that can increase the risk include:
- Inheritance pattern: Wilson’s disease is autosomal recessive, meaning a child needs one faulty gene from each parent to develop the condition.
- Carriers: If a child inherits one normal gene and one faulty gene, they are a carrier and usually show no symptoms.
Risk for carrier parents:
-
25% chance the child will have Wilson’s disease
-
50% chance the child will be a carrier
-
25% chance the child will inherit normal genes
Stay a step ahead. Book a consultation to discuss genetic testing and catch Wilson’s disease before it causes serious problems.
Diagnosis of Wilson’s Disease
Wilson's disease diagnosis involves several steps to identify copper buildup and prevent organ damage, such as:
1. Medical history and physical examination
-
Doctors first review symptoms like unexplained liver problems, tremors, mood changes, or difficulty with speech or movement.
-
A detailed eye exam using a slit lamp is done to look for Kayser–Fleischer rings.
2. Blood and urine tests
-
Liver function tests: These blood tests measure liver enzymes like alanine transaminase (ALT) and aspartate transaminase (AST) that rise with liver damage, helping detect injury caused by copper buildup.
-
INR (International Normalised Ratio) & albumin: INR checks blood clotting and albumin measures a key liver-made protein; abnormal levels show reduced liver function.
-
Ceruloplasmin: It is a protein that carries copper in the blood. Low levels suggest poor copper handling, commonly seen in Wilson disease.
-
Red blood cell count (RBC): A blood test checks for anaemia, which can occur when excess copper damages red blood cells.
-
24-hour urine copper test: This test measures the amount of copper released in urine over 24 hours; high levels strongly indicate Wilson disease.
3. Genetic testing
-
A blood test examines the ATP7B gene for changes that cause Wilson disease. This can confirm the diagnosis and help identify family members who may carry the gene.
4. Liver biopsy
-
A small liver tissue sample is taken to measure copper content. It also helps assess liver health and confirms the diagnosis when other tests are inconclusive.
5. Imaging tests
-
Brain MRI: It’s used when neurological symptoms appear and can show brain changes caused by copper buildup.
-
Ultrasound or transient elastography: These imaging tests help assess liver health, including scarring or fat buildup. They support diagnosis but cannot confirm Wilson's disease on their own.
6. Leipzig scoring system
-
Doctors may use this point-based system that combines all major findings—ceruloplasmin, eye rings, urinary/liver copper, genetic tests, and neurological signs.
-
A score of 4 or higher strongly suggests Wilson's disease, especially if individual tests are inconclusive.
Do you want reliable lab results? With Tata 1mg, getting tested is easier than ever, accurate, and hassle-free.
Prevention of Wilson’s Disease
Wilson’s disease can’t really be prevented because it’s something you inherit from your parents, but getting genetic counselling and doing family screening early makes a huge difference.
When identified early, often before symptoms appear, and treated promptly, the condition can be effectively controlled, helping prevent complications.
Doctor to Visit
While a general physician can help identify early signs of Wilson’s disease, proper management requires a multidisciplinary team, including:
- Paediatrician (in children)
- Hepatologist
- Neurologist
- Clinical geneticist
- Gastroenterologist
- Psychiatrist or psychologist
- Dietitian
- Ophthalmologist
- Physiotherapist
A paediatrician identifies early signs of Wilson disease in children—such as liver problems, behavioural changes, or poor growth—orders initial tests, and coordinates timely referral to specialists.
A hepatologist leads the treatment plan by assessing liver damage, managing copper-chelating therapy, and monitoring long-term liver health.
A neurologist treats neurological symptoms such as tremors, coordination issues, and speech or movement problems.
A clinical geneticist confirms the diagnosis, explains inheritance, and guides genetic testing for family members.
A gastroenterologist helps evaluate digestive symptoms and monitors liver-related complications.
A psychiatrist or psychologist supports emotional well-being, especially if patients experience behavioural or cognitive changes.
A dietitian guides a low-copper diet and helps maintain balanced nutrition during treatment.
An ophthalmologist examines eye changes like Kayser–Fleischer rings and monitors vision-related symptoms.
A physiotherapist develops exercises to improve strength, balance, and mobility affected by neurological issues.
When to see a doctor?
Seek medical attention if you or your child notice:
-
Tremors, slurred speech, or difficulty walking
-
Behavioural changes or mood swings
-
Persistent abdominal pain or swelling
-
Dark urine, easy bruising
-
Trouble with school performance or coordination in children
Don’t delay evaluation. Early diagnosis and treatment can prevent serious liver and neurological damage.
Treatment of Wilson’s Disease
Treatment for Wilson’s disease depends on the stage. Symptomatic treatment lowers copper quickly in people with symptoms, maintenance therapy keeps copper under control for the long term, and preventive treatment starts early in those without symptoms to stop problems before they appear.
Symptomatic treatment includes:
1. Medications
For people showing symptoms, treatment focuses on quickly reducing copper levels to prevent organ damage. Symptomatic treatment includes:
Chelation therapy (copper-removal medications):
-
Penicillamine (Cuprimine): Helps remove copper through urine; used in the initial phase.
-
Trientine hydrochloride (Syprine, Cuvrior): Removes copper via urine and faeces. It usually has fewer side effects than penicillamine
Non-chelation therapy: It Blocks copper absorption from food; preferred for long-term control and for people who never had symptoms.
Example: Zinc salts (zinc acetate, such as Galzin)
2. Liver transplantation
-
Recommended in severe or sudden liver failure when medicines no longer help.
-
It cures the disease by replacing the faulty liver. halts further disease progression.
3. Emerging therapies (still investigational, not yet standard)
Researchers are developing new treatments to help the body manage excess copper. Options include:
-
Tetrathiomolybdate (TTM) shows promising early trial results, particularly for people with neurological symptoms.
-
Gene therapy and new drugs (curcumin and stress-kinase inhibitors) are currently being investigated to correct the underlying ATP7B gene defect.
If you have long-term liver issues or high pressure in the liver, medicines like aspirin and ibuprofen can increase the risk of stomach or gut bleeding. Paracetamol is often preferred only in carefully limited doses — but only when used as advised by your doctor.
Need doctor-prescribed medicines? Order them safely from Tata 1mg with expert guidance.
Home-Care for Wilson’s Disease
Managing Wilson’s disease mainly focuses on keeping copper levels low so your liver and brain stay healthy. Along with regular treatment, a few everyday habits can help you feel better and avoid complications.
1. Diet and food choices
What you eat matters—some foods naturally contain more copper than others. Making mindful swaps can help keep copper under control. Always remember, dietary changes are a helpful extra step, not a substitute for medication.
Lower-copper foods you can include:
-
Vegetables: broccoli, cauliflower, cabbage, green beans, lettuce, carrots
-
Fruits: apples, oranges, berries, melons
-
Grains: white rice, white pasta, white bread, oat or rice cereals
-
Dairy: milk, yoghurt, cheese, non-chocolate ice cream
-
Proteins: eggs, chicken, turkey, tuna, cod, trout
-
Others: butter, oils, honey, jams, tea, coffee, fruit juices
Avoiding high-copper foods, such as:
-
Shellfish, liver, organ meats, mushrooms, nuts and seeds, chocolate, and any multivitamins that contain copper
Along with a low-copper diet, some people may also need vitamin B6 supplements as advised by their doctor. Find trusted vitamin B6 and other daily supplements on Tata 1mg.
2. Copper exposure restriction
-
Checking your drinking water—especially if you use well water—for copper content.
-
Homes with copper pipes should run tap water for a few minutes before use.
-
Avoid copper cookware or utensils, as they can release copper into food.
2. Keep your liver healthy
-
Get your hepatitis A and hepatitis B vaccines.
-
Avoid alcohol unless your doctor says it’s safe.
-
Maintain a healthy weight and stay active.
Stay protected with the right vaccines—book your adult vaccinations easily at home.
Living with Wilson’s Disease
Living with Wilson’s disease means staying consistent with treatment, caring for your emotional well-being, and keeping a close watch on your liver and copper levels. Here are some simple ways to manage daily life with this condition:
1. Stay patient and consistent with medications
- Stick to your medication regimen: Stopping treatment can allow copper to build up again, leading to serious complications.
- Taking your prescribed medicines regularly is the most important step toward staying healthy.
Need help staying consistent? Check out these 7 easy tips to stay on track with your medicines.
2. Pregnancy planning
- If you’re pregnant or planning a pregnancy, inform your doctor early.
- Your medication doses may need adjustment to keep both you and your baby safe.
Tip: Continue taking your copper-lowering medicines exactly as prescribed, and attend regular follow-ups so your doctor can track copper levels and fine-tune your treatment.
3. Emotional support
- Living with a long-term condition can bring mood changes, anxiety, or emotional stress.
- Counselling or therapy can help you cope better and stay motivated throughout treatment.
Pair emotional care with support tools. Explore doctor-approved mind-care essentials to stay calm, focused, and more in control.
4. Monitoring and supportive care
Regular check-ups are essential to confirm that copper levels are under control, treatment is working, and side effects are caught early.
How often?
-
When starting or changing treatment: monthly to quarterly visits and labs
-
Once stable: usually every 3–6 months, with a full check-up (liver tests, INR, CBC, urinalysis, and 24-h urine copper) at least twice a year
Complications of Wilson’s Disease
Wilson’s disease can affect multiple organs, with complications ranging from the liver and brain to the eyes, heart, and blood. Common complications include:
- Liver complications: People may develop fluid in the abdomen (ascites), confusion from liver dysfunction (hepatic encephalopathy), bleeding from enlarged veins (variceal bleeding), kidney issues (hepatorenal syndrome), liver cancer, or even acute liver failure.
Explore our liver care products to maintain a healthy, active life after consulting with your doctor. - Blood complications: Some people may experience anaemia (low red blood cells) or muscle injury or breakdown (rhabdomyolysis) because of excess copper in the body.
- Eye complications: Copper deposits may form Kayser-Fleischer rings or sunflower cataracts, sometimes affecting vision.
Keep your vision sharp and protected—browse our eye-care range. - Heart complications: The disease can lead to a weakened heart muscle (cardiomyopathy) or irregular heartbeats and conduction issues.
Support your heart health with trusted essentials—explore our heart-care range. - Treatment-related complications: Chelation therapy may temporarily worsen neurological symptoms before improvement, while liver transplantation can resolve severe liver-related complications.
- Nervous system complications: Copper buildup can cause tremors, stiffness (dystonia), slurred speech (dysarthria), poor coordination (ataxia), and mood or personality changes such as irritability and anxiety.
Alternative Therapies for Wilson’s Disease
Alternative therapies for Wilson’s disease can help ease symptoms, improve movement, and support day-to-day functioning. These approaches should always be used alongside prescribed copper-lowering treatment and under medical guidance.
1. Physical therapy
-
It includes gentle stretching, strengthening, balance, and coordination exercises to improve movement and reduce stiffness.
-
It helps enhance stability, muscle strength, and coordination—especially when tremors, stiffness, or walking difficulties are present.
Get exercise equipment to support physical therapy and maintain strength at home.
2. Occupational therapy
-
Focuses on making everyday tasks—like writing, dressing, or using utensils—easier by improving motor skills and teaching simple adaptive techniques.
-
Therapists may also suggest helpful devices such as special grips or supportive braces to make daily routines safer and more manageable.
3. Speech therapy
-
Beneficial for individuals dealing with speech or swallowing difficulties due to neurological involvement.
-
Speech therapists can teach exercises to improve clarity, strengthen muscles, and reduce choking risks.
4. Relaxation techniques
- Gentle practices such as yoga, breathing exercises, and mindfulness may help reduce muscle tension, improve body awareness, and support stress management—especially during long-term treatment.
Pair your relaxation routine with gentle Ayurvedic support. Browse mind-care picks here.